Aetiology
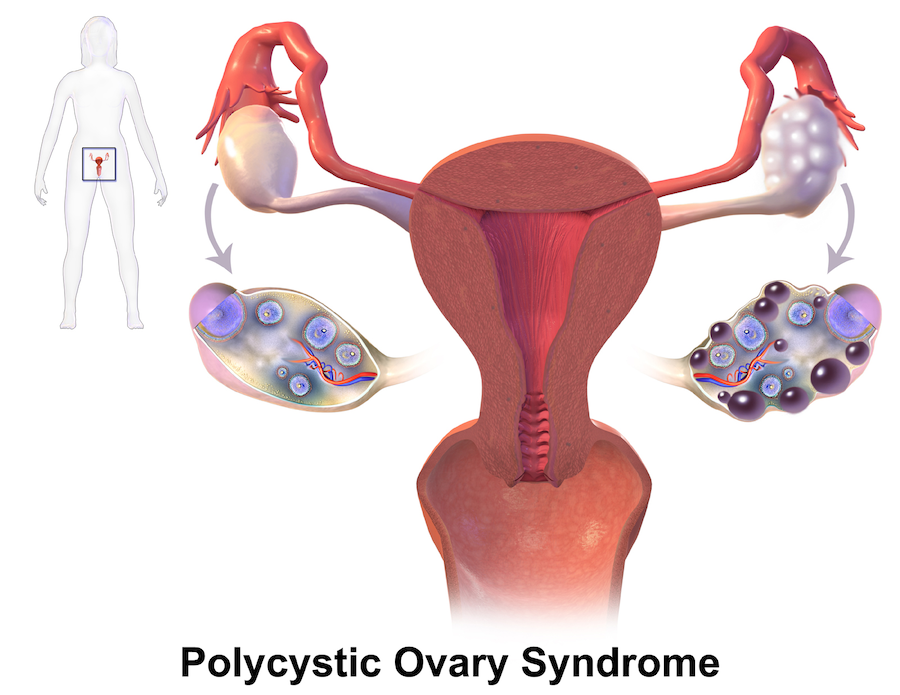
Polycystic ovarian syndrome (PCOS) is a multifactorial disorder with a complex aetiology, including the influence of genetic and environmental factors.
It features hyperandrogenism, ovarian dysfunction, and polycystic ovaries. A robust body of evidence indicates that a key pathophysiological defect is insulin resistance, which contributes to hyperinsulinemia—both of which stimulate ovarian androgen production and inhibit hepatic sex hormone-binding globulin (SHBG) production, leading to elevated free androgen levels.
Furthermore, obesity exacerbates these metabolic and reproductive abnormalities.
Risk Factors
Obesity is considered an independent risk factor for PCOS. A strong genetic predisposition has been identified, suggesting that PCOS may run in families. Other risk factors include sedentary lifestyle, unhealthy eating habits, and exposure to certain environmental toxins.
Signs and Symptoms
The clinical presentation can vary from one individual to another, but the three primary features are androgen excess, ovulatory dysfunction, and polycystic ovaries. Common manifestations include hirsutism, acne, androgenic alopecia, oligomenorrhea or amenorrhea, and anovulatory infertility.
Furthermore, women with PCOS often demonstrate various metabolic disturbances, including insulin resistance, dyslipidemia, and an increased risk of type 2 diabetes and cardiovascular disease.
Diagnosis
The diagnosis of PCOS is typically made using the Rotterdam criteria, requiring the presence of at least two of the following three features: clinical and/or biochemical hyperandrogenism, ovulatory dysfunction, and polycystic ovaries visualized on ultrasound. Clinicians must rule out other disorders of androgen excess or ovulatory dysfunction prior to confirming the diagnosis.
Dietary Recommendations
Given the links between obesity, insulin resistance, and PCOS, several dietary approaches may improve outcomes. These include a calorie-restricted diet for overweight/obese individuals, a low-glycemic-index diet, and the DASH diet (Dietary Approaches to Stop Hypertension). Moreover, integrating physical activity is usually recommended.
Treatment
Lifestyle modification remains the first-line treatment for PCOS. For reproductive-related manifestations of PCOS, hormonal contraceptives are often recommended to regulate menstrual cycles and mitigate androgen excess.
Insulin-sensitizing agents, such as metformin, are also commonly used, particularly among women with metabolic disturbances. For fertility issues, ovulation induction is typically performed. In intractable cases, surgical interventions such as laparoscopic ovarian drilling might be considered.
It must be noted that the management plan should be individualized, bearing in mind the phenotype of PCOS, the woman’s quality of life, her age, and her desire for fertility.
New Discovery: The role of kisspeptin
Kisspeptin, a neuropeptide produced in the anterior region of the hypothalamus seems to modulate the GnRH secretion and therefore the hypothalamic-hypophyseal-ovarian axis (HHO-axis) and may therefore play a significant role in PCOS.
Effects of Vitex agnus-castus in an animal model of PCOS
The study evaluated the effect of Vitex negundo L. in the letrozole-induced polycystic ovarian syndrome in rats. PCOS induced animals were treated with aqueous (Group III - 200 mg/kg and IV- 400 mg/kg) and hydroalcoholic extract (Group V- 200 mg/kg and VI- 400 mg/kg) of Vitex negundo up to 66 days.
Body weight and oestrous cycle phase were measured every day. Blood samples were collected on 0, 21 and 66 days for the measurement of fasting blood glucose, lipid profile, LH, FSH and hormonal level.
Oral glucose tolerance test was performed to study insulin resistance effect. Toxicity markers; SGOT, SGPT, and creatinine also measured at the end of the study. The administration of Letrozole led to an abnormality in serum sex steroid profile, lipid profile, glucose and oestrous cycle.
Vitex was able to successfully exert its protective effect by restoring parameters to the normal level and disappearance of cysts in ovaries. The aqueous and hydro-alcoholic extracts of seeds of Vitex negundo showed significant amelioration of Letrozole induced PCOS.
Reference: Kakadia N, Patel P, Deshpande S, Shah G. Effect of Vitex negundo L. seeds in letrozole induced polycystic ovarian syndrome. J Tradit Complement Med. 2018 Oct 11;9(4):336-345. doi: 10.1016/j.jtcme.2018.03.001. PMID: 31453130; PMCID: PMC6701941.
Another in vivo study found that vitex extract inhibited downregulation of KISS-1 gene in the hypothalamus of PCOS rats.
Because of the master role of kisspeptin in adjusting the HPG axis, vitex is likely to show beneficial effects in the treatment of PCOS via regulation of kisspeptin expression. This finding indicates a new aspect of vitex effect and may be considered in its clinical applications.
Reference: Feyzollahi Z, Mohseni Kouchesfehani H, Jalali H, Eslimi-Esfahani D, Sheikh Hosseini A. Effect of Vitex agnus-castus ethanolic extract on hypothalamic KISS-1 gene expression in a rat model of polycystic ovary syndrome. Avicenna J Phytomed. 2021 May-Jun;11(3):292-301. PMID: 34046325; PMCID: PMC8140208.
Clinical trial
A study of 14 patients with PCOS and primary or secondary infertility underwent laboratory investigations during the follicular phase of their menstrual cycles, testing for kisspeptin, luteinizing hormone (LH), follicle-stimulating hormone (FSH), oestradiol, testosterone, insulin, blood sugar levels and prolactin. An abdominal-pelvic scan and full body examination were also performed.
Patients were treated with myoinositol 750 mg/day and vitex 400 mg/day. After three months of treatment, patients agreed to have a second check-up to see if any changes occurred.
Results: The study found significant positive differences when considering kisspeptin, oestradiol, FSH and prolactin serum values. There was no significant difference in testosterone and insulin serum levels. An increase in LH serum levels was also observed.
The mean ovarian volume before treatment was 14.0 for the right ovaries and 13.8 for the left ovaries. After treatment and the recommended lifestyle changes, a decrease in the mean ovarian volume (13.5 for the right ovaries and 13.4 for the left ovaries) was noted.
Discussions and conclusions: The aetiology of PCOS, which is considered a multifactorial pathology, remains unclear. Multiple studies have been conducted and are still exploring the role of kisspeptin as an etiologic factor for PCOS associated with infertility. Our study showed a decrease in kisspeptin values after the use of myo-inositol and vitex in patients with PCOS, therefore supporting the long-standing theory that kisspeptin might have an essential role in the development of PCOS.
Reference: Akad M, Socolov D, Akad F, Covali R, Crauciuc E, Stan C, Stan C, Socolov R. Treatments in Patients with Polycystic Ovary Syndrome and Effects on Kisspeptin Serum Levels. Maedica (Bucur). 2022 Dec;17(4):799-804. doi: 10.26574/maedica.2022.17.4.799. PMID: 36818240; PMCID: PMC9923052.
Note of caution
However, naturopath and herbalist, Ruth Trickey, who is one of Australia’s most experienced practitioners with an extensive knowledge of herbal medicine for women’s health and the author of the seminarl text book, Women, Hormones and the Menstrual Cycle, has cautioned about the use of Vitex agnus-castus having observed that some women with PCOS can experience a worsening of the regularity of the menstrual cycle with vitex treatment.
This highlights the need for further research and also the necessity for invidualised prescribing.
Note also that vitex was included in the fixed Unani formulations described below.
Bibliography
The Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. (2004). Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertility and Sterility, 81, 19–25.
Legro, R.S. (2012). Obesity and PCOS: Implications for diagnosis and treatment. Seminars in Reproductive Medicine, 30(6), 496–506.Diamanti-Kandarakis, E., & Dunaif, A. (2012). Insulin Resistance and the Polycystic Ovary Syndrome Revisited: An Update on Mechanisms and Implications. Endocrine Reviews, 33 (6), 981-1030.
Nybacka, Å., Hellström, P. M., & Hirschberg, A. L. (2017). Increased fibre and reduced trans fatty acid intake are primary predictors of metabolic improvement in overweight polycystic ovary syndrome—Substudy of randomized trial between diet, exercise and diet plus exercise for weight control. Clinical endocrinology, 87(6), 680–688.
Moran, L.J., Pasquali, R., Teede, H.J., Hoeger, K.M., & Norman, R.J. (2009). Treatment of obesity in polycystic ovary syndrome: a position statement of the Androgen Excess and Polycystic Ovary Syndrome Society. Fertility and Sterility, 92(6), 1966–1982.
Azziz, R., Carmina, E., Chen, Z., Dunaif, A., Laven, J.S., Legro, R.S., Lizneva, D., Natterson-Horowtiz, B., Teede, H.J., & Yildiz, B.O. (2016). Polycystic ovary syndrome. Nature reviews Disease primers, 2, 16057.
Key herbal medicines in PCOS
- Actaea racemosa
- Asperagus racemosus
- Chamaelirium luteum
- Cinnamomum verum
- Curcuma longa
- Glycyrrhiza spp.
- Humulus lupulus
- Nigella sativa
- Paeonia lactiflora
- Tribulus terrestris
- Trigonella foenum-graecum
- Vitex agnus-castus
Studies and Reviews
Naturopathic clinician, Dr Susan Arentz, conducted a systemic review in 2017 as part of her PhD. She also led a clinical trial examining a combination of lifestyle modification and herbal medicines for PCOS (described below).
Systematic Review by Dr Arentz
Nutritional supplements and herbal medicines for women with polycystic ovary syndrome; a systematic review and meta-analysis.
This systematic review examined the effect of herbal and nutritional supplements on menstrual regulation and adverse effects in women with PCOS. Results showed no evidence of improved menstrual regularity or reduced amenorrhoea, and mild adverse effects were found for Cinnamomum sp. compared to placebo.
Twenty-four studies (1406 women) investigating seven nutritional supplements and four herbal medicines were included. No one study was assessed as having a low risk of bias. Four trials reported on the primary endpoint menstrual regulation.
There was no evidence on improved menstrual regularity for calcium plus vitamin D compared to Metformin
(RR: 0.66, 95% CI 0.35 to 1.23, p = 0.19), reduced amenorrhoea for Camellia sinensis compared to placebo (RR: 0.17, 95% CI 0.02 to 1.72, p = 0.13) and no difference in the number of menses per month for Cinnamomum sp. against placebo (MD 0.05, 95% CI -0.36 to 1.36, p = 0.26).
Adverse effects were investigated in seven studies (164 women). Mild adverse effects were found for Cinnamomum sp. compared to placebo (17 women, RR: 0.36, 95% CI 0.03 to 0.70, p = 0.03).
No difference was found for adverse effects between inositol, B complex vitamins, vitamin D, chromium and placebo. Improved reproduction, metabolic hormones and hyperandrogenism was found for inositol and improved cholesterol for omega three fish oils.
Conclusion: There is no high-quality evidence to support the effectiveness of nutritional supplements and herbal medicine for women with PCOS and evidence of safety is lacking. High quality trials of nutritional supplements and herbal medicines examining menstrual regulation and adverse effects in women with PCOS are needed
Reference
Arentz, S., et al. (2017). "Nutritional supplements and herbal medicines for women with polycystic ovary syndrome; a systematic review and meta-analysis." BMC Complement Altern Med 17(1): 500.
https://pubmed.ncbi.nlm.nih.gov/29178904
Free PDF : https://bmccomplementmedtherapies.biomedcentral.com/counter/pdf/10.1186/s12906-017-2011-x.pdf
Combined Lifestyle and Herbal Medicine in Overweight Women with Polycystic Ovary Syndrome (PCOS): A Randomized Controlled Trial.
This randomized controlled trial provided evidence of improved effectiveness and safety for lifestyle intervention when combined with herbal medicines in women with PCOS.
Methods
The lifestyle intervention was based on evidence-based guidelines for the management of PCOS, which recommend a calorie-controlled diet and exercise for at least 150 minutes per week.
The herbal intervention consisted of two tablets.
Tablet 1 contained Cinnamomum verum, Glycyrrhiza glabra, Hypericum perforatum, and Paeonia lactiflora.
Tablet 2 contained Tribulus terrestris. The primary outcome was oligomenorrhoea/amenorrhoea. Secondary outcomes were hormones; anthropometry; quality of life; depression, anxiety and stress; pregnancy; birth outcomes; and safety.
Results
At 3 months, women in the combination group recorded a reduction in oligomenorrhoea of 32.9% (95% confidence interval 23.3–42.6, p < 0.01) compared with controls. Other significant improvements were found for body mass index (p < 0.01); insulin (p = 0.02) and luteinizing hormone (p = 0.04); blood pressure (p = 0.01); quality of life (p < 0.01); depression, anxiety and stress (p < 0.01); and pregnancy rates (p = 0.01).
Conclusion
The study concluded that lifestyle intervention when combined with herbal medicines improved effectiveness and safety in women with PCOS. The combination group recorded a significant reduction in oligomenorrhoea and improvements in body mass index, insulin and luteinizing hormone levels, blood pressure, quality of life, depression, anxiety, stress, and pregnancy rates.
Reference
Arentz, S., et al. (2017). "Combined Lifestyle and Herbal Medicine in Overweight Women with Polycystic Ovary Syndrome (PCOS): A Randomized Controlled Trial." Phytother Res 31(9): 1330-1340.
https://pubmed.ncbi.nlm.nih.gov/28685911
Other reviews
Herbal Remedies for PCOS
This literature review discusses the diagnosis, signs, symptoms, causes, and risk factors of PCOS, as well as the role of Glycyrrhiza glabra, Aloe vera, Silybum marianum, Serenoa repens, Actaea racemosa, and Angelica sinensis in its management.
Reference
Zeng, L. H., et al. (2022). "Polycystic Ovary Syndrome: A Disorder of Reproductive Age, Its Pathogenesis, and a Discussion on the Emerging Role of Herbal Remedies." Front Pharmacol 13: 874914. https://pubmed.ncbi.nlm.nih.gov/35924049
The Role of medicinal herbs in treatment of insulin resistance in patients with Polycystic Ovary Syndrome: A literature review
This review investigates the role of medicinal herbs in treating PCOS, finding that Aloe vera, cinnamon, green tea, fenugreek, and silymarin may be beneficial.
Reference
Ashkar, F., et al. (2020). "The Role of medicinal herbs in treatment of insulin resistance in patients with Polycystic Ovary Syndrome: A literature review." Biomol Concepts 11(1): 57-75. https://pubmed.ncbi.nlm.nih.gov/34233418
Herbal Remedies for Polycystic Ovary Syndrome
Herbal medicines can improve symptoms of Polycystic Ovary Syndrome (PCOS) with minimal side effects and a longer treatment cycle.
The review of the literature showed that plants such as aloe vera and chamomile improve fertility by increasing the number of ovarian follicles. Besides, Vitex agnus-castus reduce hirsutism by reducing testosterone and androgen levels. It was also shown that liquorice, ginseng, cinnamon, and Inositol improve the adverse effects of diabetes caused by PCOS by lowering lipid and blood glucose levels.
Moreover, Stachys lavandulifolia (wood betony) and fennel are effective in changing endometrial tissue parameters in PCOS by reducing estrogen and hyperplasia.
Reference
Manouchehri, A., et al. (2023). "Polycystic ovaries and herbal remedies: A systematic review." JBRA Assist Reprod 27(1): 85-91. https://pubmed.ncbi.nlm.nih.gov/35916457
Polycystic ovaries and herbal remedies: A systematic review.
This review focussed on the use of herbal remedies to treat polycystic ovary syndrome (PCOS). It found that aloe vera, chamomile, Vitex agnus-castus, liquorice, ginseng, cinnamon, de chiro Inositol, Stachys lavandulifolia, and fennel can improve fertility, reduce hirsutism, and lower lipid and blood glucose levels.
Reference
Manouchehri, A., et al. (2023). "Polycystic ovaries and herbal remedies: A systematic review." JBRA Assist Reprod 27(1): 85-91.
Fixed combination Picolin
Fixed combination Picolin (Cinnamomum verum, Glycyrrhiza glabra, Linum usitatissimum, Vitex agnus castus)
A prospective, double-blind, placebo controlled, parallel-group, multi-centre clinical trial of 217 women with PCOS found that vitex extract BNO 1095 significantly reduced symptoms. No serious adverse event (SAE) occurred in either group.
The mean total PMSD score decreased from 29.23 at baseline (0 cycle) to 6.41 at the termination (3rd cycle) for the treatment group and from 28.14 at baseline (0 cycle) to 12.64 at the termination (3rd cycle) for the placebo group. The total PMSD score of 3rd cycle was significantly lower than the baseline in both groups (p<0.0001). The difference in the mean scores from the baseline to the 3rd cycle in the treatment group (22.71+/-10.33) was significantly lower than the difference in the placebo group (15.50+/-12.94, p<0.0001). Results of PMTS were similar, the total scores for PMTS were significantly lower between the two groups (p<0.01) and within each group (p<0.01). The score was decreased from 26.17+/-4.79 to 9.92+/-9.01 for the treatment group, and from 27.10+/-4.76 to 14.59+/-10.69 for the placebo group. A placebo effect of 50% was found in the present study (Ishaq et al. 2021).
Another study found that a Unani herbal formulation (Picolin) containing Cinnamomum verum, Glycyrrhiza glabra, Linum usitatissimum, Vitex agnus castus was comparatively more effective than metformin in reducing serum insulin and prolactin. The improvement in the menstrual flow in the PCOS patients after treatment with either capsule Picolin, tablet Picolin-E or metformin were improved by 84%, 61% and 54%, respectively (Hameed, Farooq, and Qureshi 2021).
References
Hameed, L., A. D. Farooq, and T. Qureshi. 2021. 'Analysis of Unani coded formulation on the hormonal parameters of patients with polycystic ovarian syndrome', Pak J Pharm Sci, 34: 899-907.
Ishaq, S., H. Rizwani G, H. Shareef, S. Fatima, H. Anser, and S. Sarfraz. 2021. 'A herbal treatment approach for the management of clinical, hormonal and ultrasound parameters in reproductive age group women with polycystic ovarian syndrome: A randomized clinical trial', Pak J Pharm Sci, 34: 1097-102.
Nigella
A Review of Clinical and Preclinical Studies on the Therapeutic Potential of Black Seeds (Nigella sativa) in the Management of Polycystic Ovarian Syndrome (PCOS).
This review article focuses on the potential of Nigella sativa to manage women with PCOS. Several clinical and preclinical studies have demonstrated that the major bioactive constituent of black seed (N. sativa), thymoquinone, has potential for managing women with PCOS.
Reference
Balasubramanian, R., et al. (2023). "A Review of Clinical and Preclinical Studies on the Therapeutic Potential of Black Seeds (Nigella sativa) in the Management of Polycystic Ovarian Syndrome (PCOS)." J Pharmacopuncture 26(1): 1-9.
https://pubmed.ncbi.nlm.nih.gov/37007297
Herbal medicine for the management of polycystic ovary syndrome (PCOS) and associated oligo/amenorrhoea and hyperandrogenism; a review of the laboratory evidence for effects with corroborative clinical findings.
This narrative review examines the reproductive endocrine effects in PCOS for an alternative treatment, herbal medicine. Eighteen pre-clinical studies reported mechanisms of effect and fifteen clinical studies corroborated pre-clinical findings, including eight randomised controlled trials, and 762 women with menstrual irregularities, hyperandrogenism and/or PCOS. Interventions included herbal extracts of Vitex agnus-castus, Cimicifuga racemosa, Tribulus terrestris, Glycyrrhiza spp., Paeonia lactiflora and Cinnamomum cassia.
Reference
Arentz, S., et al. (2014). "Herbal medicine for the management of polycystic ovary syndrome (PCOS) and associated oligo/amenorrhoea and hyperandrogenism; a review of the laboratory evidence for effects with corroborative clinical findings." BMC Complement Altern Med 14: 511. https://pubmed.ncbi.nlm.nih.gov/25524718
Black cohosh
This prospective randomized controlled trial studied the role of Cimicifuga racemosa extract in ovulation induction in women with PCOS. Results showed favourable changes in LH level and FSH/LH ratio, higher progesterone level and endometrial thickness, and higher pregnancy rate in the Klimadynon group.
Reference
Kamel, H. H. (2013). Role of phyto-oestrogens in ovulation induction in women with polycystic ovarian syndrome. Eur J Obstet Gynecol Reprod Biol 168(1): 60-63. https://pubmed.ncbi.nlm.nih.gov/23347605
Cinnamon
Cinnamon improves metabolic factors without detectable effects on adiponectin in women with polycystic ovary syndrome.
This double-blind randomized controlled clinical trial investigated the effects of cinnamon supplementation on glycemic indices, serum lipids and adiponectin in patients with polycystic ovary syndrome (PCOS). Results showed that cinnamon significantly decreased serum fasting blood glucose, insulin, homeostatic model assessment for insulin resistance, total cholesterol and low-density lipoprotein cholesterol and weight and increased high-density lipoprotein cholesterol compared with placebo.
Reference
Borzoei, A., et al. (2018). "Cinnamon improves metabolic factors without detectable effects on adiponectin in women with polycystic ovary syndrome." Asia Pac J Clin Nutr 27(3): 556-563. https://pubmed.ncbi.nlm.nih.gov/29737802.
Insulin resistance improvement by cinnamon powder in polycystic ovary syndrome: A randomized double-blind placebo controlled clinical trial.
This randomized double-blind placebo-controlled clinical trial assesses the effect of cinnamon powder capsules on insulin resistance, anthropometric measurements, glucose and lipid profiles, and androgens of women with polycystic ovarian syndrome (PCOS). Results suggest that cinnamon significantly reduced fasting insulin and insulin resistance in women with PCOS.
Reference
Hajimonfarednejad, M., et al. (2018). "Insulin resistance improvement by cinnamon powder in polycystic ovary syndrome: A randomized double-blind placebo controlled clinical trial." Phytother Res 32(2): 276-283. https://pubmed.ncbi.nlm.nih.gov/29250843 Free PDF : https://onlinelibrary.wiley.com/doi/10.1002/ptr.5970
The effect of cinnamon supplementation on glycemic control in women with polycystic ovary syndrome: A systematic review and meta-analysis.
This review provides comprehensive information about the effect of cinnamon on insulin resistance (IR) indices in women with PCOS. Results indicated that cinnamon supplementation significantly reduced homeostatic model assessment for insulin resistance (HOMA-IR) scores.
Reference
Heshmati, J., et al. (2021). "The effect of cinnamon supplementation on glycemic control in women with polycystic ovary syndrome: A systematic review and meta-analysis." J Food Biochem 45(1): e13543. https://pubmed.ncbi.nlm.nih.gov/33111340
Effects of cinnamon on controlling metabolic parameters of polycystic ovary syndrome: A systematic review and meta-analysis
This systematic review and meta-analysis of clinical trials found that cinnamon supplementation may help PCOS patients to manage their metabolic parameters, with significant decreases in fasting blood sugar, fasting insulin, and HOMA-IR, as well as reductions in LDL-C, total cholesterol, and triacylglycerol.
Reference
Heydarpour, F., et al. (2020). "Effects of cinnamon on controlling metabolic parameters of polycystic ovary syndrome: A systematic review and meta-analysis." J Ethnopharmacol 254: 112741. https://pubmed.ncbi.nlm.nih.gov/32151755
Shatavari
Impact of Stress on Female Reproductive Health Disorders: Possible Beneficial Effects of Shatavari (Asparagus racemosus)
This review examines the potential beneficial effects of shatavari (Asparagus racemosus) on female reproductive health disorders caused by stress. It proposes that shatavari may improve female reproductive health complications including hormonal imbalance, polycystic ovarian syndrome (PCOS), follicular growth and development, oocyte quality and infertility possibly by reducing oxidative stress and increasing antioxidants level in the body.
Reference
Pandey, A. K., et al. (2018). "Impact of stress on female reproductive health disorders: Possible beneficial effects of shatavari (Asparagus racemosus)." Biomed Pharmacother 103: 46-49. https://pubmed.ncbi.nlm.nih.gov/29635127
Curcumin
Effect of Curcumin on Glycaemic and Lipid Parameters in Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
This systematic review and meta-analysis of five randomized controlled trials found that curcumin administration in PCOS resulted in significant improvement in glycaemic parameters, but no significant changes were seen in lipid parameters.
Reference
Simental-Mendía, L. E., et al. (2022). "Effect of Curcumin on Glycaemic and Lipid Parameters in Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis of Randomized Controlled Trials." Reprod Sci 29(11): 3124-3133.
https://pubmed.ncbi.nlm.nih.gov/34655047
Therapeutic effect and safety of curcumin in women with PCOS: A systematic review and meta-analysis
This review aimed to evaluate the efficacy and safety of curcumin in the treatment of PCOS. Results showed that curcumin decreased body mass index, fasting plasma glucose, insulin, homeostatic model assessment for insulin resistance, total cholesterol, and C-reactive protein, and increased the quantitative insulin sensitivity check index. Curcumin has beneficial effects on serum markers of inflammation, weight loss and glucose and lipid metabolism in patients with PCOS.
Reference
Shen, W., et al. (2022). "Therapeutic effect and safety of curcumin in women with PCOS: A systematic review and meta-analysis." Front Endocrinol (Lausanne) 13: 1051111. https://pubmed.ncbi.nlm.nih.gov/36387924
The effects of curcumin as dietary supplement for patients with polycystic ovary syndrome: An updated systematic review and meta-analysis of randomized clinical trials.
This systematic review concluded that among patients with PCOS, the use of curcumin demonstrated a significant difference from the control group for glycaemic control, suggesting that curcumin confers clinical benefits in patients with PCOS.
Reference
Abdelazeem, B., et al. (2022). "The effects of curcumin as dietary supplement for patients with polycystic ovary syndrome: An updated systematic review and meta-analysis of randomized clinical trials." Phytother Res 36(1): 22-32.
https://pubmed.ncbi.nlm.nih.gov/34517426
Therapeutic Effect of Curcumin in Women with Polycystic Ovary Syndrome Receiving Metformin: A Randomized Controlled Trial
This RCT showed that curcumin has a synergistic effect with metformin in the improvement of insulin resistance and lipid profile in patients with PCOS.
Reference
Sohrevardi, S. M., et al. (2021). "Therapeutic Effect of Curcumin in Women with Polycystic Ovary Syndrome Receiving Metformin: A Randomized Controlled Trial." Adv Exp Med Biol 1308: 109-117. https://pubmed.ncbi.nlm.nih.gov/33861440
The Role of medicinal herbs in treatment of insulin resistance in patients with Polycystic Ovary Syndrome: A literature review.
This narrative review aimed to investigate the role of herbal substances on the treatment of PCOS. Results indicate that some medicinal herbs may have a key role in treating PCOS. Natural substances such as Aloe vera, cinnamon, green tea, fenugreek, and silymarin can be used as a new supportive care for PCOS.
Reference
Ashkar, F., et al. (2020). "The Role of medicinal herbs in treatment of insulin resistance in patients with Polycystic Ovary Syndrome: A literature review." Biomol Concepts 11(1): 57-75. https://pubmed.ncbi.nlm.nih.gov/34233418
Pomegranate juice
The effect of concentrated pomegranate juice consumption on risk factors of cardiovascular diseases in women with polycystic ovary syndrome: A randomized controlled trial.
This randomized clinical trial examined the effects of concentrated pomegranate juice consumption on risk factors of cardiovascular diseases in women with polycystic ovary syndrome. Results showed that CPJ consumption had a beneficial effect on blood pressure, serum concentrations of TG and HDL-C, and TG/HDL-C ratio.
Reference
Abedini, M., et al. (2021). "The effect of concentrated pomegranate juice consumption on risk factors of cardiovascular diseases in women with polycystic ovary syndrome: A randomized controlled trial." Phytother Res 35(1): 442-451.
Salvia miltiorrhiza
The Effects of Salvia miltiorrhiza on Reproduction and Metabolism in Women with Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis.
This systematic review and meta-analysis of 6 RCTs suggests that Salvia miltiorrhiza extract has beneficial effects on reproduction and glucose and lipid metabolism in women with PCOS, and is generally safe for clinical application.
Reference
Shen, W., et al. (2021). "The Effects of Salvia miltiorrhiza on Reproduction and Metabolism in Women with Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis." Evid Based Complement Alternat Med 2021: 9971403.
Tribulus
Tribulus terrestris and female reproductive system health: A comprehensive review.
This review discussed in detail the beneficial impact of Tribulus terrestris L. and its secondary metabolites on the female reproductive system. 23 articles were found, which approved the efficacy of T. terrestris on improvements in histological features of the ovary and uterus, enhancements in the sexual desire of postmenopausal syndrome, and improvements in ovarian and breast cancers.
Reference
Ghanbari, A., et al. (2021). "Tribulus terrestris and female reproductive system health: A comprehensive review." Phytomedicine 84: 153462. https://pubmed.ncbi.nlm.nih.gov/33602600
Image credit: BruceBlaus, CC BY-SA 4.0 , via Wikimedia Commons